What You Should Know About Hyperlipidemia
Healthline
What is hyperlipidemia?
Hyperlipidemia is a medical term for abnormally high levels of fats (lipids) in the blood. The two major types of lipids found in the blood are triglycerides and cholesterol.
Triglycerides are made when your body stores the extra calories it doesn’t need for energy. They also come directly from your diet in foods such as red meat and whole-fat dairy. A diet high in refined sugar, fructose, and alcohol raises triglycerides.
Cholesterol is produced naturally in your liver because every cell in your body uses it. Similar to triglycerides, cholesterol is also found in fatty foods like eggs, red meat, and cheese.
Hyperlipidemia is more commonly known as high cholesterol. Although high cholesterol can be inherited, it’s more often the result of unhealthy lifestyle choices.
Understanding cholesterol
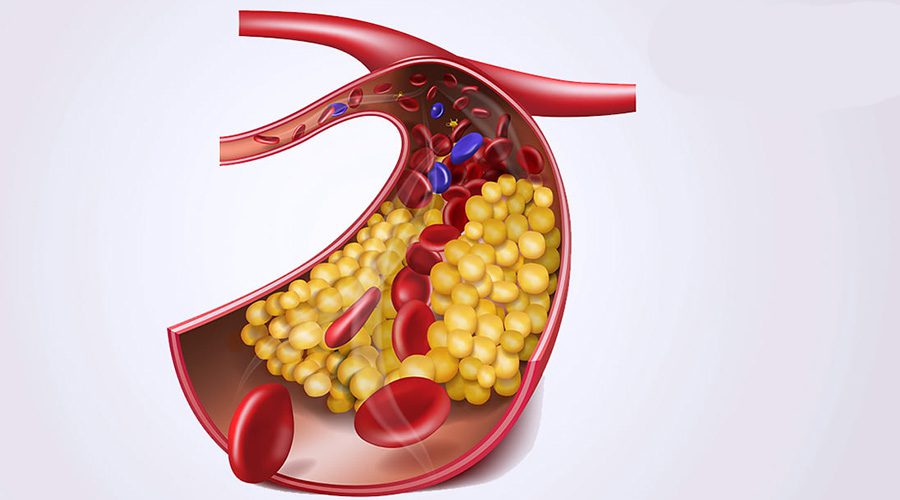
Cholesterol is a fatty substance that travels through your bloodstream on proteins called lipoproteins. When you have too much cholesterol in your blood, it can build up on the walls of your blood vessels and form plaque. Over time, plaque deposits grow larger and begin to clog up
your arteries, which can lead to heart disease, heart attack, and stroke.
Getting a diagnosis
Hyperlipidemia has no symptoms, so the only way to detect it is to have your doctor perform a blood test called a lipid panel or a lipid profile.
This test determines your cholesterol levels.
Your doctor will take a sample of your blood and send it to a lab for testing, then get back to you with a full report. Your report will show your levels of:
- total cholesterol
- low-density lipoprotein (LDL) cholesterol
- high-density lipoprotein (HDL) cholesterol
- triglycerides
Your doctor may ask you to fast for 8 to 12 hours before getting your blood drawn. That means you’ll need to avoid eating or drinking anything other than water during that time.
However, recent studies suggest that fasting isn’t always necessary, so follow your doctor’s instructions in regard to your particular health concerns.
Generally, a total cholesterol level above 200 milligrams per deciliter is considered high.
However, safe levels of cholesterol can vary from person to person depending on health history and current health concerns, and are best determined by your doctor. Your doctor will use your lipid panel to make a hyperlipidemia diagnosis.
Are you at risk for hyperlipidemia?
There are two types of cholesterol, LDL and HDL. You’ve probably heard them called “bad” and “good” cholesterol, respectively.
LDL (“bad”) cholesterol builds up in your artery walls, making them hard and narrow.
HDL (“good”) cholesterol cleans up excess “bad” cholesterol and moves it away from the arteries, back to your liver.
Hyperlipidemia is caused by having too much LDL cholesterol in your blood and not enough HDL cholesterol to clear it up.
Unhealthy lifestyle choices can raise “bad” cholesterol levels and lower “good” cholesterol levels. If you’re overweight, eating lots of fatty foods, smoking, or not getting enough exercise, then you’re at risk.
Lifestyle choices that put you at risk for high cholesterol include:
- eating foods with saturated and trans fats
- eating animal protein, like meat and dairy
- not getting enough exercise
- not eating enough healthy fats
- obesity
- large waist circumference
- smoking
- drinking alcohol excessively
Abnormal cholesterol levels are also found in some people with certain health conditions, including:
- kidney disease
- diabetes
- polycystic ovary syndrome
- pregnancy
- underactive thyroid
- inherited conditions
As well, your cholesterol levels may be affected by certain medications: • birth control pills
- diuretics
- some depression medications
Familial combined hyperlipidemia
There’s a type of hyperlipidemia that you can inherit from your parents or grandparents. It’s called familial combined hyperlipidemia. Familial combined hyperlipidemia causes high cholesterol and high triglycerides.
People with this condition often develop high cholesterol or high triglyceride levels in their teens and receive a diagnosis in their 20s or 30s.
This condition increases the risk of early coronary artery disease and heart attack.
Unlike people with typical hyperlipidemia, people with familial combined hyperlipidemia may experience symptoms of cardiovascular disease after a few years, such as:
- chest pain (at a young age)
- heart attack (at a young age)
- cramping in the calves while walking
- sores on the toes that don’t heal properly
- stroke symptoms, including trouble speaking, drooping on one side of the face, or weakness in the extremities
How to treat and manage hyperlipidemia at home
Lifestyle changes are the key to managing hyperlipidemia at home.
Even if your hyperlipidemia is inherited (familial combined hyperlipidemia), lifestyle changes are still an essential part of treatment. These changes alone may be enough to reduce your risk of complications like heart disease and stroke.
If you’re already taking medications, lifestyle changes can improve their cholesterol lowering effects.
Eat a heart-healthy diet
Making changes to your diet can lower your “bad” cholesterol levels and increase your “good” cholesterol levels. Here are a few changes you can make:
• Choose healthy fats. Avoid saturated fats that are found primarily in red meat, bacon, sausage, and full-fat dairy products. Choose lean proteins like chicken, turkey, and fish when possible. Switch to low-fat or fat-free dairy. And use monounsaturated fats like olive and canola oil for cooking.
• Cut out the trans fats. Trans fats are found in fried food and processed foods, like cookies, crackers, and other snacks. Check the ingredients on product labels. Skip any product that lists “partially hydrogenated oil.”
• Eat more omega-3s. Omega-3 fatty acids have many heart benefits. You can find them in some types of fish, including salmon, mackerel, and herring. They can also be found in some nuts and seeds, like walnuts and flax seeds.
• Increase your fiber intake. All fiber is heart-healthy, but soluble fiber, which is found in oats, brain, fruits, beans, and vegetables, can lower your LDL cholesterol levels.
• Learn heart-healthy recipes. Check out the American Heart Association’s recipe page for tips on delicious meals, snacks, and desserts that won’t raise your cholesterol.
• Eat more fruits and veggies. They’re high in fibre and vitamins and low in saturated fat.
Lose weight
If you’re overweight or obese, losing weight can help lower your total cholesterol levels. Even 5 to 10 pounds can make a difference.
Losing weight starts with figuring out how many calories you’re taking in and how many you’re burning. It takes cutting 3,500 calories from your diet to lose a pound.
To lose weight, adopt a low-calorie diet and increase your physical activity so that you’re burning more calories than you’re eating. It helps to cut out sugary drinks and alcohol, and practice portion control.
Get active
Physical activity is important for overall health, weight loss, and cholesterol levels. When you aren’t getting enough physical activity, your HDL cholesterol levels go down. This means there isn’t enough “good” cholesterol to carry the “bad” cholesterol away from your arteries.
You only need 40 minutes of moderate to vigorous exercise three or four times a week to lower your total cholesterol levels. The goal should be 150 minutes of exercise total each week. Any of the following can help you add exercise to your daily routine:
- Try biking to work.
- Take brisk walks with your dog.
- Swim laps at the local pool.
- Join a gym.
- Take the stairs instead of the elevator.
- If you use public transportation, get off a stop or two sooner.
Quit smoking
Smoking lowers your “good” cholesterol levels and raises your triglycerides. Even if you haven’t been diagnosed with hyperlipidemia, smoking can increase your risk of heart disease. Talk to your doctor about quitting or try the nicotine patch.
Hyperlipidemia medications
If lifestyle changes aren’t enough to treat your hyperlipidemia, your doctor may prescribe medication. Common cholesterol- and triglyceride-lowering medications include:
- statins, such as:
– atorvastatin (Lipitor)
– fluvastatin (Lescol XL)
– lovastatin (Altoprev)
– pitavastatin (Livalo)
– pravastatin (Pravachol)
– rosuvastatin (Crestor)
– simvastatin (Zocor) - bile-acid-binding resins, such as:
– cholestyramine (Prevalite)
– colesevelam (WelChol)
– colestipol (Colestid) - cholesterol absorption inhibitors, such asezetimibe (Zetia)
- injectable medications, such as alirocumab (Praluent) or evolocumab (Repatha)
- fibrates, like fenofibrate (Fenoglide, Tricor, Triglide) or gemfibrozil (Lopid)
- niacin (Niacor)
- omega-3 fatty acid supplements
- other cholesterol-lowing supplements
Outlook
People with untreated hyperlipidemia have a greater chance of getting coronary heart disease than the general population. Heart disease is a condition in which plaque builds up inside the coronary (heart) arteries. Hardening of the arteries, called atherosclerosis, happens when plaque builds up on the walls of arteries. Over time, plaque build-up narrows the arteries and can block them completely, preventing normal blood flow. This can lead to heart attack, stroke, or other problems.
How to prevent high cholesterol
You can make changes to your lifestyle to prevent high cholesterol or reduce your risk of developing hyperlipidemia:
- Exercise several days per week.
- Eat a diet low in saturated and trans fats.
- Include lots of fruits, vegetables, beans, nuts, whole grains, and fish regularly into your diet. (The Mediterranean diet is an excellent heart-healthy eating plan.)
- Stop eating red meat and processed meats like bacon, sausage, and cold cuts. • Drink skim or low-fat milk.
- Maintain a healthy weight.
- Eat lots of healthy fats, like avocado, almonds, and olive oil.